Claim Reimbursement Review Appeal Process FAQs
This file provides detailed instructions on the OptumRx claim reimbursement review and appeals process for pharmacy providers. It outlines the necessary steps for efficient reimbursement requests. This is an essential resource for enrolled Tennessee pharmacy providers seeking to navigate the claims process.
Edit, Download, and Sign the Claim Reimbursement Review Appeal Process FAQs
Form
eSign
Add Annotation
Share Form
How do I fill this out?
To fill out the Claim Reimbursement Review/Appeal Form, ensure you have the required documents ready. Start by downloading and completing the form accurately. Follow the instructions provided for submitting it through the OptumRx Provider Portal.
How to fill out the Claim Reimbursement Review Appeal Process FAQs?
1
Download the Claim Reimbursement Review/Appeal Form.
2
Complete the form with accurate information and required documents.
3
Create or log into your OptumRx Provider Portal account.
4
Upload the completed form through the MAC Appeal tab.
5
Submit and await written confirmation of the outcome.
Who needs the Claim Reimbursement Review Appeal Process FAQs?
1
Pharmacy providers in Tennessee need this form to request reimbursement reviews.
2
Providers seeking clarity on claim adjudications will benefit from this form.
3
Audit departments of pharmacies will use this process for reimbursement accountability.
4
Healthcare administrators require it for maintaining financial accuracy in pharmacy claims.
5
Pharmacy accountants will utilize this form for effective record-keeping of claims.
How PrintFriendly Works
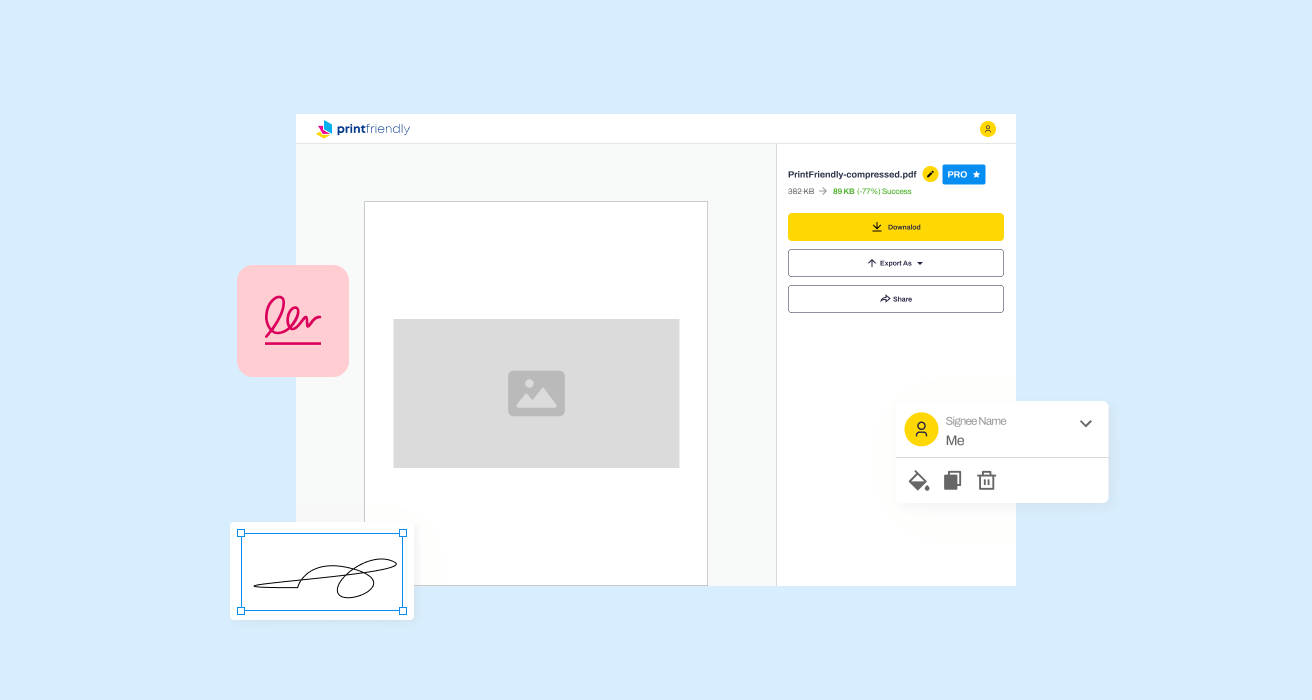
At PrintFriendly.com, you can edit, sign, share, and download the Claim Reimbursement Review Appeal Process FAQs along with hundreds of thousands of other documents. Our platform helps you seamlessly edit PDFs and other documents online. You can edit our large library of pre-existing files and upload your own documents. Managing PDFs has never been easier.
Edit your Claim Reimbursement Review Appeal Process FAQs online.
Editing this PDF on PrintFriendly is simple and user-friendly. You can modify text, reorganize pages, and add new content as needed. Our editor provides all the tools required to customize your document seamlessly.
Add your legally-binding signature.
With PrintFriendly, signing your PDF is straightforward. Utilize our signature feature to add your signature directly within the document. This ensures your document is professional and legally compliant.
Share your form instantly.
Sharing your PDF on PrintFriendly is easy. You can quickly generate a shareable link or use email options to send your document directly to others. This feature enhances collaboration and accessibility.
How do I edit the Claim Reimbursement Review Appeal Process FAQs online?
Editing this PDF on PrintFriendly is simple and user-friendly. You can modify text, reorganize pages, and add new content as needed. Our editor provides all the tools required to customize your document seamlessly.
1
Open the PDF in the PrintFriendly editor.
2
Select the section you wish to edit.
3
Make the needed changes using the editing tools.
4
Preview the document to see how changes look.
5
Download the edited PDF or share it directly.

What are the instructions for submitting this form?
To submit the Claim Reimbursement Review/Appeal Form, visit the OptumRx Provider Portal and log in with your credentials. Upload the completed form through the MAC Appeal tab. If you have questions, email Provider.Relations@Optum.com or call the support hotline for assistance.
What are the important dates for this form in 2024 and 2025?
Ensure timely submissions for the Claim Reimbursement Review/Appeal Form. Key dates include the start of the fiscal year in 2024, where changes may take effect. Always verify updated deadlines annually to avoid any issues.

What is the purpose of this form?
The Claim Reimbursement Review/Appeal Form serves as a necessary tool for pharmacy providers seeking remedies for unsatisfactory reimbursement outcomes. It ensures that providers can contest claims efficiently and transparently. The form guides users through the process of requesting reviews and appeals.
Tell me about this form and its components and fields line-by-line.
- 1. Provider Information: This field captures essential details about the pharmacy provider submitting the request.
- 2. Claim Details: Here, providers enter specifics regarding the claim in question.
- 3. Supporting Documentation: This field prompts users to include any relevant invoices or documents.
- 4. Signature: A signature is required to authenticate the submission of the form.
- 5. Date Submitted: This field must indicate the date on which the form is submitted.
What happens if I fail to submit this form?
Failure to submit this form may result in delayed reimbursement and unresolved claims. It is crucial to ensure all information is accurate and submitted within the specified time frame to avoid complications.
- Delayed Payments: Missing submissions can lead to significant delays in payment for services rendered.
- Inaccurate Records: Not submitting the form may lead to discrepancies in financial records.
- Unresolved Claims: Claims may remain unresolved without proper submission of appeal requests.
How do I know when to use this form?
- 1. Claim Dispute: Use this form to dispute an unfavorable claim adjudication.
- 2. Price Review: Employ the form to request a review of the reimbursement price offered.
- 3. Adjudication Clarification: It is also applicable for seeking clarification on the claim adjudication process.
Frequently Asked Questions
How do I download the Claim Reimbursement Review/Appeal Form?
You can download the form directly from the OptumRx website or through the provided links in the documentation.
What is the deadline for submitting a reimbursement request?
Requests must be submitted within seven business days of the claim's adjudication date.
Can I edit the Claim Reimbursement Review/Appeal Form?
Yes, you can edit the form using our PDF editing tools available on PrintFriendly.
What should I include with my reimbursement request?
Ensure to include a completed form and relevant invoice documentation for the appeal.
How will I know if my appeal has been accepted?
OptumRx will send a written response indicating the outcome within seven business days.
Can I contact OptumRx for help?
Yes, you can contact OptumRx for assistance at their dedicated phone number or email.
Is there a specific format for the invoices?
Invoices must match the NDC on the pharmacy claim and be dated appropriately.
How do I create an account on the OptumRx Portal?
Visit the OptumRx Provider Portal and follow the instructions to create a new account.
What if my appeal is denied?
You will receive a written response explaining the denial, along with possible alternatives.
What kinds of claims are automatically denied?
Duplicate claims and certain reimbursement types like AWP or FUL will result in automatic denials.
Related Documents - OptumRx Claims Process
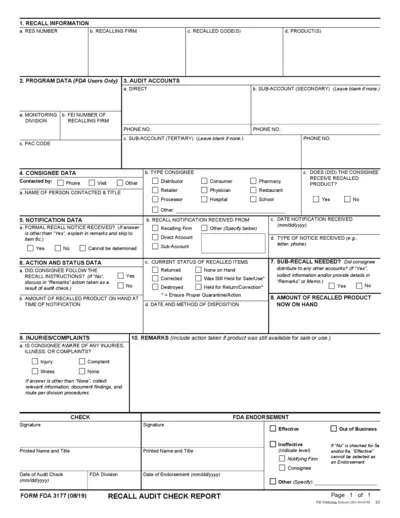
FDA Recall Audit Check Report Instructions
This file provides detailed instructions for completing the FDA Recall Audit Check Report. It includes information on recall details, program data, audit accounts, and consignee data. Useful for those involved in managing FDA recalls.
Assessment of Abuse Potential of Drugs Guidance for Industry
This document provides guidance for the assessment of abuse potential in drugs. It covers key decision points, recommended studies, and the process for NDA submission. This is crucial for ensuring drug safety and regulatory compliance.
Nurtec ODT Savings Program Terms & Conditions
This document provides detailed terms and conditions for the Nurtec ODT Savings Program. It includes eligibility criteria, instructions for pharmacists, and important disclaimers. Patients using the copay card should adhere to these guidelines to benefit from the program.
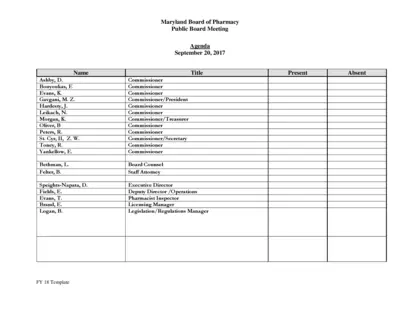
Maryland Board of Pharmacy Public Board Meeting Agenda
This file contains the agenda for the Maryland Board of Pharmacy's public board meeting on September 20, 2017. It includes reports from various committees and updates on operations, licensing, compliance, and more. The document is essential for stakeholders to keep track of board activities and decisions.
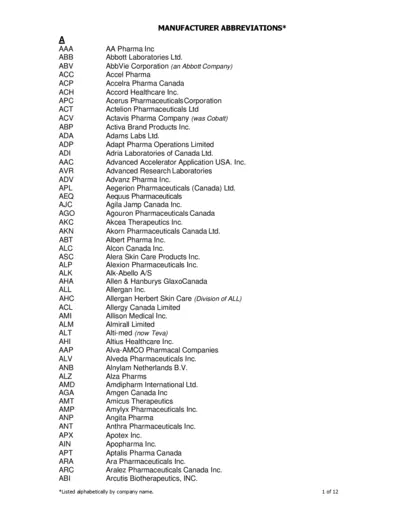
Abbreviations for Pharma Manufacturers
This file contains a list of manufacturers' abbreviations organized alphabetically, helping users to identify manufacturer names and their corresponding abbreviations.
Pharma-Lagom: Safe and Effective Medication Use
Pharma-Lagom is a comprehensive guide on the risks and benefits of medication use, aimed at promoting safe and effective medication practices. It includes contributions from experts in the Pharmacy Department of Kalaniketan Polytechnic College, Jabalpur. This document also covers recent events and achievements within the department.
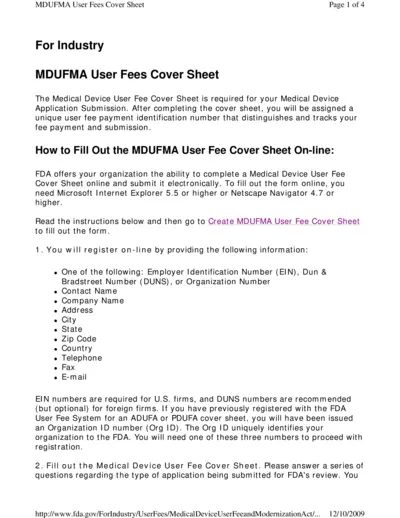
MDUFMA User Fees Cover Sheet Instructions
The MDUFMA User Fees Cover Sheet is required for Medical Device Application Submission. It includes details on registration and payment processes. Follow this guide to complete and submit your form correctly.
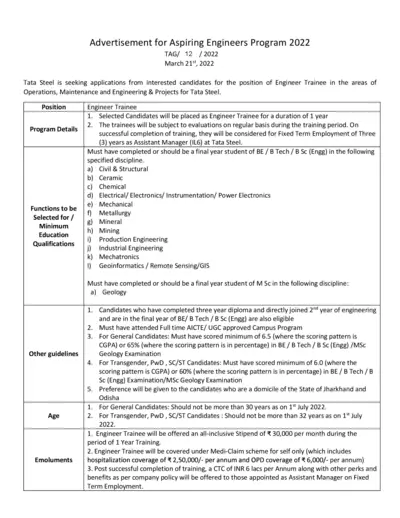
Tata Steel Aspiring Engineers Program 2022 Application
This file includes details about Tata Steel's Aspiring Engineers Program 2022. It covers program details, eligibility criteria, and the application process. It also provides information on evaluation, guidelines, and submission deadlines.
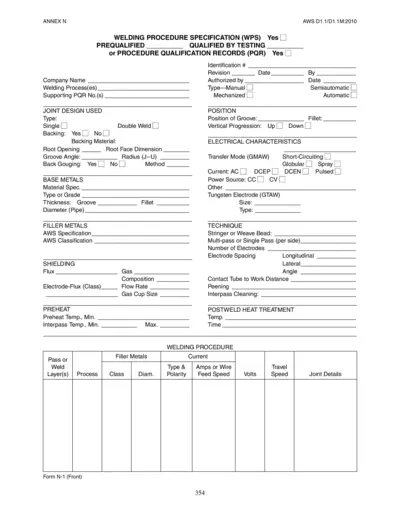
Welding Procedure Specification (WPS) PDF Guide
This file is a Welding Procedure Specification (WPS) that provides detailed instructions for welding procedures, joint design, base metals, filler metals, and more. It includes sections for prequalified and qualified-by-testing procedures. This document is essential for ensuring weld quality and consistency.
California Intern Pharmacist Application Instructions
This document provides detailed instructions for applying for an Intern Pharmacist license in California. It covers processing time, required materials, and special cases for expedited review. Ensure all requirements are met to avoid application delays.

Botox Cosmetic Patient Medication Information
This file contains detailed information about Botox Cosmetic (onabotulinumtoxinA). It includes dosage, administration, warnings, precautions, and adverse reactions. The document is intended for healthcare professionals and patients.

Join the Kings Club and Save Instantly with a Kings Club Card
Apply for a Kings Club Card at any of our locations and start saving instantly. Fill out the form in-store or online to receive your card. Enjoy discounts and additional benefits with your Kings Club membership.