Medicare/Medicaid Documents
Medicare/Medicaid
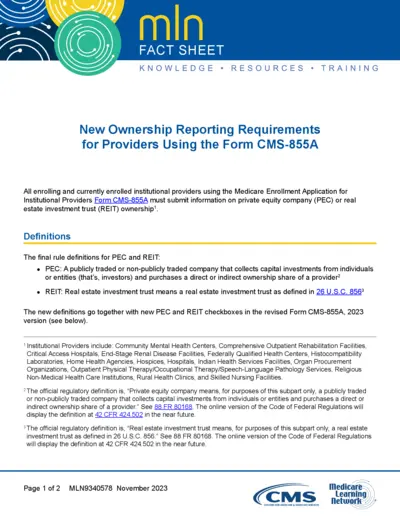
New Ownership Reporting Requirements for CMS-855A
This file outlines the new ownership reporting requirements for providers using Form CMS-855A. It includes details about private equity company and real estate investment trust ownership. Providers must understand the new definitions and reporting guidelines to ensure compliance.
Medicare/Medicaid
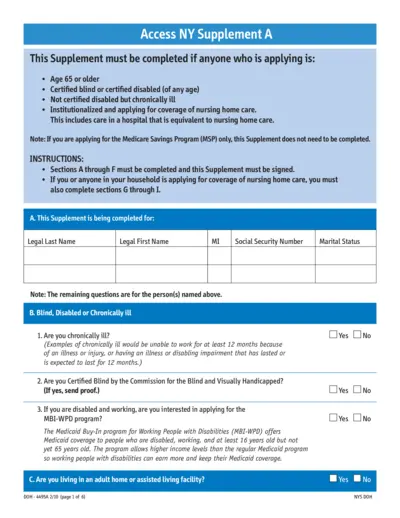
Access NY Supplement A Application Instructions
This file provides detailed instructions for completing the Access NY Supplement A application. It specifically targets individuals who are applying based on age, blindness, or disability. Proper completion of this document is essential for qualifying for Medicaid-related services.
Medicare/Medicaid
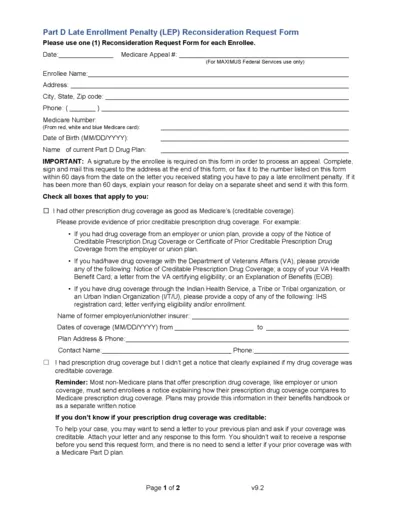
Medicare Part D Late Enrollment Penalty Reconsideration
This file provides the Late Enrollment Penalty Reconsideration Request Form for Medicare beneficiaries. It outlines how to fill out the form and the necessary documentation needed for an appeal. It is essential for those seeking to contest a late enrollment penalty.
Medicare/Medicaid
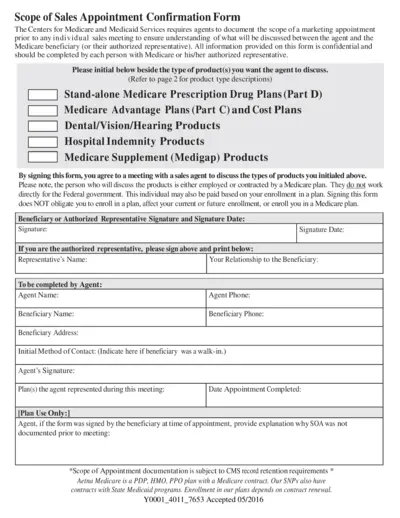
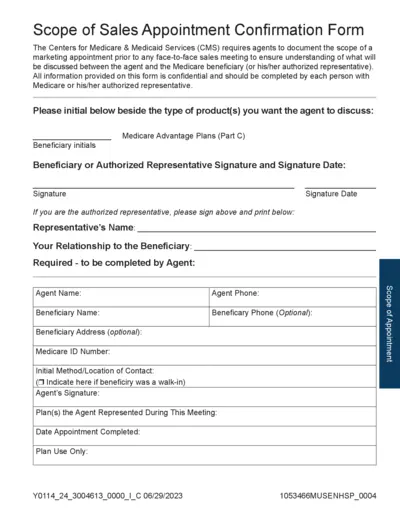
Scope of Sales Appointment Confirmation Form
This form documents the scope of a marketing appointment for Medicare sales meetings. It ensures both the agent and the Medicare beneficiary understand the discussion topics. All information is confidential and must be signed by the beneficiary or their authorized representative.
Medicare/Medicaid
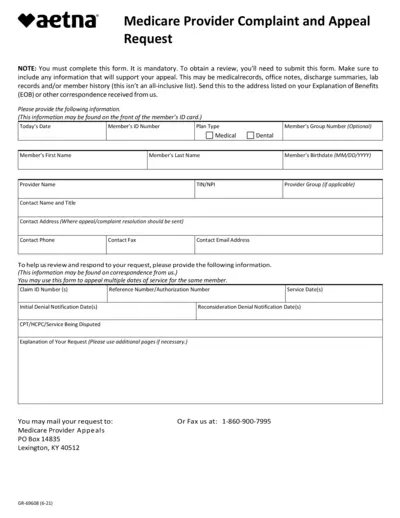
Medicare Provider Complaint and Appeal Form
This file is essential for members wishing to appeal decisions made by Medicare. It provides a structured way to gather the necessary information for a successful appeal. Completing this form ensures that your concerns are heard and addressed promptly.
Medicare/Medicaid
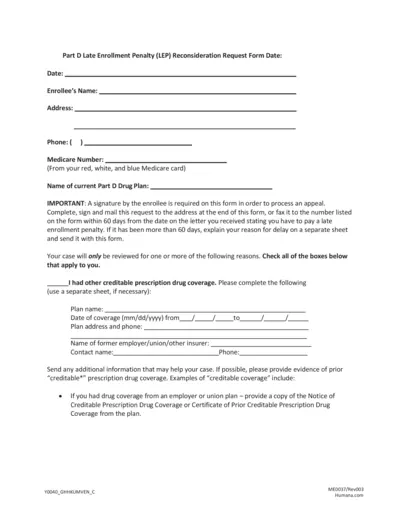
Part D Late Enrollment Penalty Reconsideration Request
This file contains the Late Enrollment Penalty Reconsideration Request Form for Medicare beneficiaries. It provides necessary instructions for completing the appeal process. Users can find key information regarding eligibility and required documentation.
Medicare/Medicaid
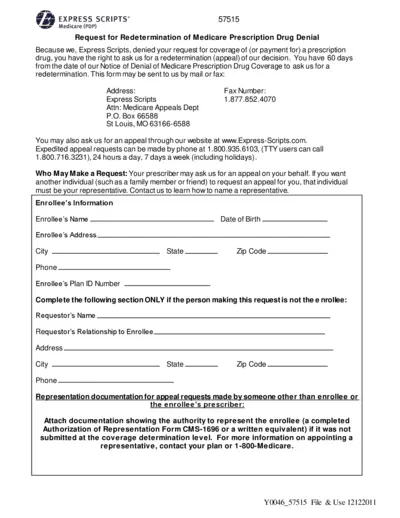
Request for Medicare Prescription Drug Coverage Redetermination
This form is used to appeal a denial of coverage for a Medicare prescription drug. Users have 60 days from the notice of denial to request a redetermination. It's essential for enrolled patients needing coverage reconsideration for their medications.
Medicare/Medicaid
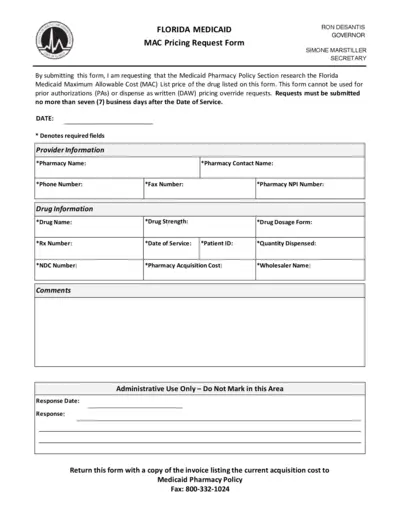
Florida Medicaid MAC Pricing Request Form
This form is used to request the Florida Medicaid Pharmacy Policy Section to research the MAC list price for a specified drug. It includes important details required for submission. Proper completion ensures timely processing of your request.
Medicare/Medicaid
Medicare Sales Appointment Confirmation Form
This form is essential for documenting a Medicare sales appointment. It ensures that both agents and beneficiaries are aligned on the discussed topics. Use this form to protect sensitive information and streamline your appointment process.
Medicare/Medicaid
Guide to Enrolling in Medicare Part A and B
This file provides essential information on enrolling in Medicare, focusing on Part A and Part B details. It outlines eligibility, enrollment periods, and how to access Medicare services. Navigate this booklet for comprehensive guidance and support.

Medicare/Medicaid
Advance Beneficiary Notice of Non Coverage Guidelines
This document provides guidelines on filling out the Advance Beneficiary Notice (ABN). It outlines eligibility for Medicare coverage and the importance of the ABN form. Understanding this file ensures proper billing and patient responsibility.
Medicare/Medicaid
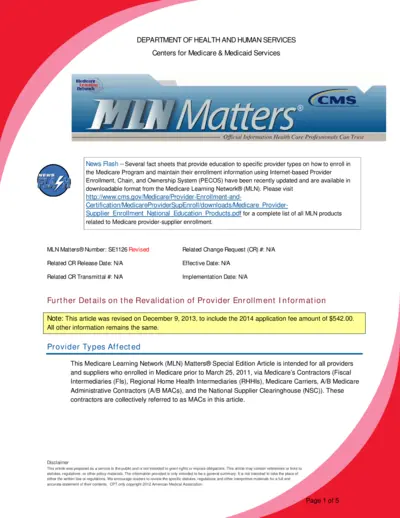
Medicare Provider Enrollment Revalidation Guide
This file contains updated information for Medicare providers regarding the enrollment revalidation process. It includes essential details about requirements and processes to ensure compliance. Providers must understand these guidelines to maintain their enrollment effectively.